Do you struggle with addictive tendencies? Do you find yourself only able to complete things when there’s a deadline in place, procrastinate over boring tasks but equally get caught up in things that are enjoyable to you? Almost to the point of obsession! It may be that you are one of the 2 to 4% of adults that have ADHD.
I have worked in the field of addiction for over 30 years and have been a qualified addiction therapist for 25 of those years. I remember hearing the term ADHD for the first time almost 30 years ago. It was from a friend who had just been diagnosed with it. To be honest I thought it was a nicer way of calling someone an attention seeker! I was also really worried that it could be used as a way of minimising addiction. Over 30 years later and thankfully I’ve learnt so much more about both addiction and ADHD. It turns out that ADHD has nothing to do with attention seeking and everything to do with struggling to keep your attention focused on things that are either difficult or somewhat boring and challenging to you.
Have you ever had a school report that said ‘…… does not concentrate’? Disclaimer: ADHD does not mean you didn’t do well in school or can’t become a high achiever. It probably does mean that if you found a subject challenging and that subject didn’t ‘light you up’ that you would have found it very difficult to focus and concentrate on it.
Have you ever been called a daydreamer? Daydreaming is a way of dissociating from difficult tasks and is very common with people with ADHD. Neuro typical persons also daydream. They also procrastinate and can become obsessive over enjoyable things. When you add risky, impulsive behaviours such as addiction into the mix you are possibly looking at ADHD. It can be difficult to know what’s what because so many ADHD symptoms are also things that most of the population struggle with from time to time. Having ADHD means you have less dopamine than a Neuro typical person thus are more likely to get your ‘feel goods’ from addictive behaviours such a substance use, gambling or sex addiction. (We could substitute the aforementioned addictions for workaholism, gym addiction, shopping addiction, food addiction, phone addiction etc). All the above hit the pleasure reward spot in the brain – the part of the brain that creates and releases dopamine. If you have less dopamine than what is considered the normal amount it then makes sense that you may keep returning to a behaviour that stimulates those feel good chemicals. In time that behaviour may turn into an addiction. Addiction is when that behaviour no longer feels like a choice. You begin to feel obsessed and compelled to carry out that behaviour. You begin to ‘act out’ in order to feel ok.
Many of my clients have to make a choice between controlled use of their addiction or abstinence from it. Every client is different and needs a different course of treatment. It is my role to explore with my clients whether they can control their ‘use’ or not. What I have found is that those clients who present with ADHD symptoms do not always fit into the classic mold of the ‘addict’. And by that I mean that they are able to have control of their use at some points rather than the 12 step philosophy that states that more often than not when someone takes that first drink/drug/gamble/bit of sugar etc – it will set off a physical compulsion and a mental obsession to consume/act out more. Those with ADHD may actually have addictive tendencies rather than be struggling with addiction. Therefore if the correct diagnosis and treatment is sought and given they may be able to have control over their use in the future. It is only through a comprehensive assessment – exploring a person’s past experiences that a plan of action can be agreed. Many of my clients have both ADHD and addiction in which case abstinence may well be the only way forward.
For a full addiction assessment please get in touch via email at Victoriaabadi66@gmail.com
For an ADHD assessment please contact your GP or private specialist ADHD consultant psychiatrist.

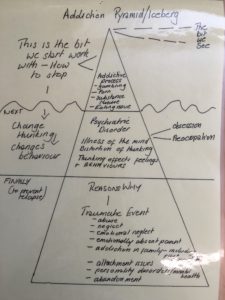 Over the years I have devised a three tiered way of working with clients. Think of an iceberg divided into 3 parts. The top part of the iceberg is the bit that clients usually present in therapy with. They come to me stating that they are obsessively and compulsively using a substance or addictive behaviour, such as gambling or watching pornography. If they are using a substance such as alcohol or cocaine daily then the first thing we need to work on is stopping that behaviour so that they can become psychologically available for counselling. At this point the work that I may be doing with the client may look and feel more like advice and guidance rather than therapy. This is the bit that is visible. We will look at what support the client can access, what are the barriers to them accessing that support. Helping the client understand that life has to be better clean and sober than it is using or drinking. This looks and feels different to every individual but in my experience has to be about connection to their life and others in some meaningful form or other. It may be a connection to other recovering people, a connection with a hobby such as yoga, running or painting. Again this is more effective in making the client have a sense of wellbeing if they are connected to others practicing/participating in the same thing. I remember one of my clients describing to me the importance of having found her tribe. She had tried the 12 step model of attending mutual aid meetings but had not felt comfortable with this. She went on to use therapy weekly combined with yoga for the next 12 months. Within her yoga practice she met a lot of other likeminded people. She felt connected. She had found a place where she felt she belonged. Addiction more often than not takes a person to a place of isolation. I now understand isolation to be something born from a sense of shame and self-loathing. It doesn’t start out that way. It starts out as using substances on your own primarily so as to not be seen to using too much, not having to explain yourself, an underlying sense that the way your using is not quite right, maybe a sense of paranoia if other people are around, it may even be you just don’t want to have to share your stash. Whatever the reasons may start out as somewhere along the line something changes. That desire to be alone turns into a need to be alone. Facing other people becomes too difficult whether it be due to shame, embarrassment, social anxiety, depression, paranoia, psychosis and the result is the same – addicts spend more and more time alone due to need not want.
Over the years I have devised a three tiered way of working with clients. Think of an iceberg divided into 3 parts. The top part of the iceberg is the bit that clients usually present in therapy with. They come to me stating that they are obsessively and compulsively using a substance or addictive behaviour, such as gambling or watching pornography. If they are using a substance such as alcohol or cocaine daily then the first thing we need to work on is stopping that behaviour so that they can become psychologically available for counselling. At this point the work that I may be doing with the client may look and feel more like advice and guidance rather than therapy. This is the bit that is visible. We will look at what support the client can access, what are the barriers to them accessing that support. Helping the client understand that life has to be better clean and sober than it is using or drinking. This looks and feels different to every individual but in my experience has to be about connection to their life and others in some meaningful form or other. It may be a connection to other recovering people, a connection with a hobby such as yoga, running or painting. Again this is more effective in making the client have a sense of wellbeing if they are connected to others practicing/participating in the same thing. I remember one of my clients describing to me the importance of having found her tribe. She had tried the 12 step model of attending mutual aid meetings but had not felt comfortable with this. She went on to use therapy weekly combined with yoga for the next 12 months. Within her yoga practice she met a lot of other likeminded people. She felt connected. She had found a place where she felt she belonged. Addiction more often than not takes a person to a place of isolation. I now understand isolation to be something born from a sense of shame and self-loathing. It doesn’t start out that way. It starts out as using substances on your own primarily so as to not be seen to using too much, not having to explain yourself, an underlying sense that the way your using is not quite right, maybe a sense of paranoia if other people are around, it may even be you just don’t want to have to share your stash. Whatever the reasons may start out as somewhere along the line something changes. That desire to be alone turns into a need to be alone. Facing other people becomes too difficult whether it be due to shame, embarrassment, social anxiety, depression, paranoia, psychosis and the result is the same – addicts spend more and more time alone due to need not want.